In the area of Microbial testing most simply talk about mould and only to a genius level i.e aspergillus and Penicilium but what you may not know is that there is approximately 180 species of Aspergillus, but less than 40 of them are known to cause infections in humans and there are 350 identified species of Penicillium, so when someone reports you have 3,000 penicillium it doesn’t actually tell if that number if made up of 100 different species or just 1.
Here at Mycotox we know its important to identify the mould species as different species can have different impacts on humans, so we look at the common water damaged species as we know they will be the ones we find in a water damaged building.
Our testing form mould is carried out using Next generation Sequencing which identifies the mould to the species level and the levels at that site.
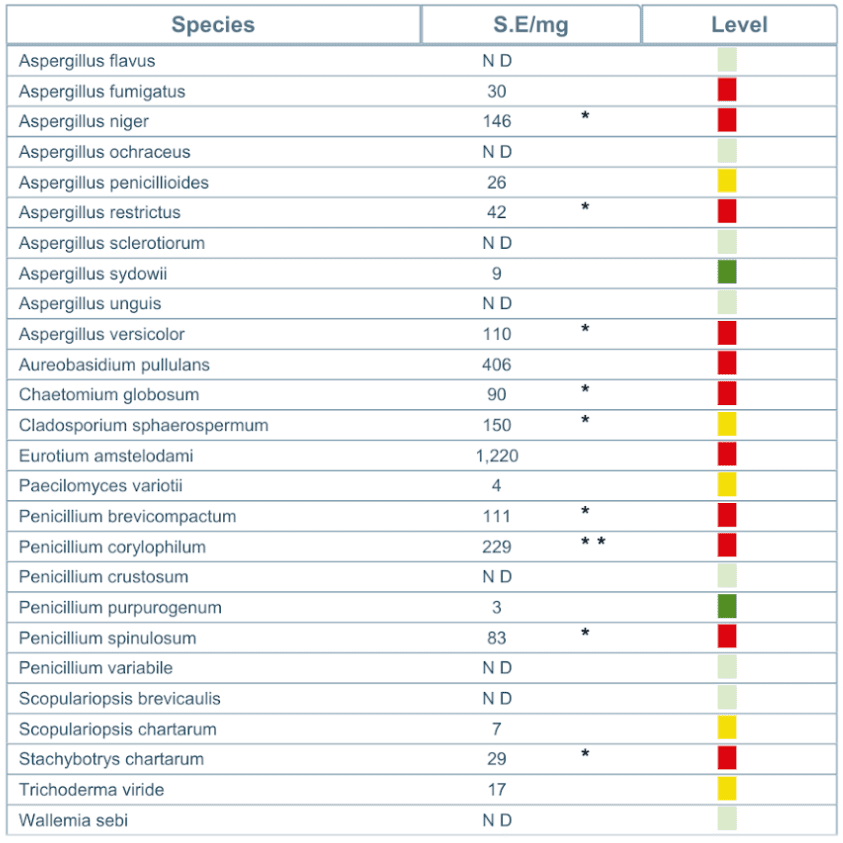
The table below represents the absolute abundance of Each Water Damage Mould Species detected in the sample reported.
(Species Equivalent per milligram (SE/mg)).
The RED Levels below show excessive levels of contamination.
With gene expression testing now showing that 70% of those with CIRS, it’s the bacteria which is the cause of their Chronic inflammatory response, with 42% due to actinomyces bacterial species and 28% due to bacterial endotoxins. So understanding what types of bacterial species you have in your contaminated home becomes extremely important. So we look to marine bacteria as naturally they thrive in a moist wet environment.
As part of understanding what impact the occupants have on the bacterial load in the home, we provide a complete profile of the human habitat bacteria- these are the ones that come from the human skin and other human activities.
As research progresses we now understand that blue-green algae is air borne and in a water-damaged building it multiples, resulting in high levels of Cyanobacteria (blue green algae). Current research is linking exposure to Cyanobacteria with Motor Neurone disease.
So any testing that does not cover the bacterial species in a contaminated building maybe missing what is causing the illness known as CIRS.